纵隔子宫(septate uterus,SU)是一种先天性子宫畸形(congenital uterine anomaly,CUA),育龄妇女的患病率约为0.2%~2.3%[1],具有较高的不孕、流产和早产的风险,而妊娠期宫颈功能不全(uterine cervical incompetence)也是其流产和早产的原因之一。应用经阴道宫颈环扎术治疗完全性SU并双宫颈双阴道及宫颈功能不全而成功抱婴回家的病例罕见报告,现报告1例原发性不孕,宫腔镜下行子宫纵隔切除术后,妊娠中期流产1次,本次孕14周经预防性宫颈环扎术,早产顺产成功抱婴回家的诊治经过,并回顾国内外相关文献。
1 病例报告
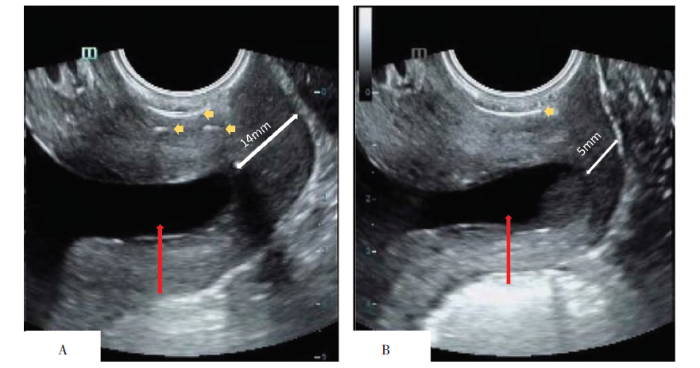
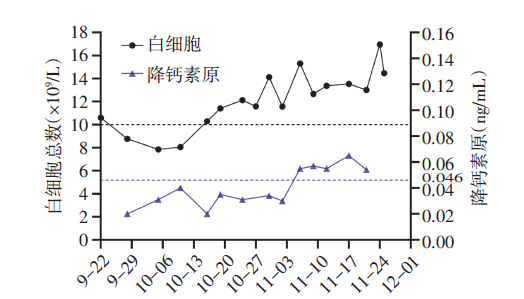
患者 女,28岁,孕2产0。因停经21+2周,宫颈环扎术后7周余,发现宫颈管缩短3 h,于2020年9月22日10:30急诊收入广州医科大学附属第三医院(我院)。患者既往体健,平素月经规律。2016年因不孕症就诊于我院,三维超声造影确诊为完全性SU,2017年9月于我院行宫腔镜下子宫纵隔切除术。2019年7月自然妊娠,孕24周流产1次。2020年1月于我院行宫腔镜检查,发现宫颈9号扩宫棒通过无阻力,诊断为宫颈功能不全。此次妊娠为自然受孕,末次月经2020年4月26日,预产期2021年2月2日。2020年7月30日孕14周以完全性SU术后、宫颈功能不全,在我院行预防性宫颈环扎术,术中见双阴道,左侧阴道长约9 cm,见一宫颈长约1.5 cm,宫口松,可容一指,Ⅰ度柱状上皮外移(见图1-1A);右侧阴道长约7 cm,见一宫颈长约1 cm,宫口松,可容一指(见图1-1B)。予MB66缝线于左侧宫颈行双层环扎,右侧宫颈单层环扎,术后观察3 d出院。术前1 d和术后3 d的左侧宫颈管超声图像见图2A、2B。出院后定期产检,胎儿Ⅲ级超声、口服葡萄糖耐量试验等均未见异常。2020年9月22日随访超声检查示:宫颈环扎术后,两侧宫颈内口均扩张,左侧剩余宫颈长为14 mm,左侧羊膜囊突入宫颈管,右侧剩余宫颈长5 mm,右侧羊膜囊可见突入宫颈管,双侧宫颈管超声图像见图3A、3B。遂急诊入院。
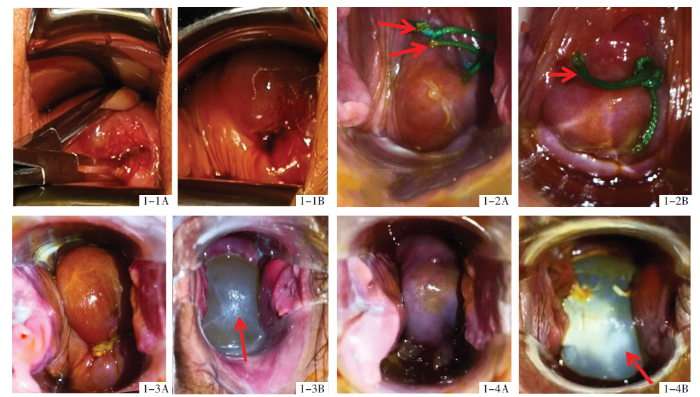
图1
图1
环扎术前后、不同孕周双侧宫颈肉眼变化图
注:1-1 为孕14周环扎术前宫颈图;1-2 为环扎术后孕15+2周宫颈图,箭头指示分别为环扎缝线(左侧双层环扎,右侧单层环扎);1-3 为环扎术后孕23+6周羊膜囊突出宫颈图,箭头指示为羊膜囊突出;1-4 为孕30+1周早产临产拆线后宫颈图,箭头指示为羊膜囊突出。其中A代表左侧宫颈,B代表右侧宫颈。
图2
图2
宫颈环扎术前、后左侧宫颈管二维超声对比图
注:A 2020年7月29日宫颈环扎术前,B 2020年8月3日宫颈环扎术后;红色箭头所示为宫颈长度,白色箭头所示为环扎线距宫颈外口长度,黄色箭头所示为环扎线强回声。
图3
图3
2020年9月22日双侧宫颈管变化超声对比图
注:A 行单线宫颈环扎术的左侧宫颈管,B 行双线宫颈环扎的右侧宫颈管;红色箭头所示为羊膜囊突入宫颈管,白色箭头所示为剩余宫颈管长度,黄色箭头所示为环扎线强回声。
妊娠前体质量40 kg,妊娠前体质量指数17.74 kg/m2,妊娠期体质量增加5 kg。入院查体:宫高17 cm,腹围75 cm,未扪及明显宫缩,胎心136次/min。阴道窥诊:左、右侧宫口均闭合,分别见2条和1条宫颈环扎线仍在原位。血常规示:白细胞10.59×109/L,快速C反应蛋白0.86 mg/L,降钙素原0.02 ng/mL。阴道分泌物培养阴性。白带常规示:白细胞(++),清洁度Ⅲ度。入院诊断:①先兆流产;②宫颈功能不全(宫颈环扎术后);③SU并双宫颈双阴道;④孕2产0,孕21+2周单活胎;⑤子宫纵隔电切术后。
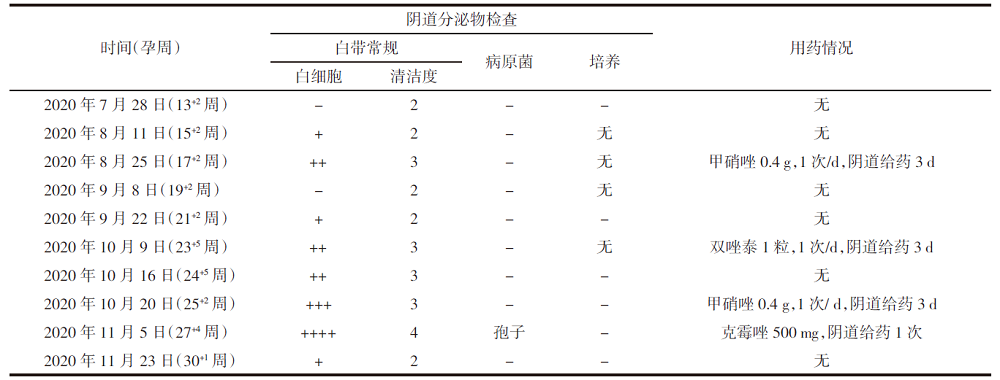
入院初始患者无自觉宫缩,予以黄体酮凝胶90 mg,1次/d,塞肛;硝苯地平10 mg,2次/d,口服,抑制宫缩治疗,定期监测宫颈长度变化,见表1。孕23+6周阴道窥视见右侧宫颈口羊膜囊突出1 cm(见图1-3B),持续加用阿托西班静脉滴注8 mL/h抑制宫缩。孕24周及27+3周分别予肌内注射地塞米松(6 mg,间隔12 h 1次,共2 d)促胎肺成熟2个疗程。孕24周、27+6周、29+6周分别用苯唑西林2 g,2次/d,静脉滴注;拉氧头孢2 g,2次/d,静脉滴注;头孢孟多1.5 g,2次/d,静脉滴注预防感染,疗程3 d。白细胞、降钙素原变化趋势见图4。宫颈环扎前后阴道分泌物情况及用药情况见表2。11月23日2:30孕30+1周诉不规则宫缩明显,增加阿托西班滴速至16 mL/h,并加静脉滴注硫酸镁1.5 g/h,进行新生儿脑保护治疗,患者仍下腹坠胀感加剧,宫缩渐规律,间隔5~8 min宫缩1次,持续20~50 s,遂完整拆除宫颈环扎线(共3条)(见图1-4A、1-4B)。患者妊娠期环扎术前、术后及其随孕周双侧宫颈肉眼变化见图1。拆线后宫缩进行性增强,难以抑制,停止滴注阿托西班,拆线后约11 h,顺产一活女婴,Apgar评分10分-10分-10分,体质量1 320 g。产后出血180 mL,分娩后检查双侧宫颈无裂伤(见图5),产后转重症新生儿科监护37 d出院,母女随访至今,健康良好。
表1 宫颈长度变化表 降钙素原(ng/mL)
| 时间(孕周) | 宫颈剩余长度 (左/右,mm) | 宫颈形态 (左/右) | 宫颈内口宽度 (左/右,mm) | 宫颈内口深度 (左/右,mm) |
|---|---|---|---|---|
| 2020年9月22日(21+2周) | 14/5 | U/U | 12/12 | 27/32 |
| 2020年9月28日(22+1周) | 12/5 | U/U | 13/10 | 27/31 |
| 2020年10月15日(24+4周) | 10/0 | U/全程扩张 | 23/- | 25/- |
| 2020年10月25日(26周) | 15/0 | Y/全程扩张 | 10/- | 33/- |
| 2020年11月3日(27+2周) | 9/0 | Y/全程扩张 | 20/- | 28/- |
图4
图5
2 讨论
2.1 SU的临床特点及对妊娠的影响
本例患者第1次妊娠中期流产,本次妊娠虽孕14周行预防性宫颈环扎,积极抗早产治疗,仍在孕30+1周早产,妊娠结局与国内外文献报道一致。
2.2 SU患者的围生育期保健
2.2.1 SU患者的妊娠前治疗
CUA的治疗主要是纠正与梗阻性症状相关的解剖异常,以缓解疼痛等症状,从而提高生活质量,避免长期影响健康和生殖导致的不良后果[9]。目前治疗SU的首选方法为宫腔镜下宫腔成形术或宫腔镜下子宫纵隔切除术[10]。目前尚无大样本的随机对照试验证明手术治疗对改善SU的不良妊娠结局有效[11]。2014年一项Meta分析显示,与未接受治疗的SU患者相比,接受宫腔镜下子宫纵隔切除术的妊娠早中期患者自然流产率降低(RR=0.37,95%CI:0.25~0.55),而2组的妊娠率(RR=1.14,95%CI:0.79~1.65)和早产率(RR=0.66,95%CI:0.29~1.49)差异无统计学意义[12]。
本例患者术前备孕2年未孕,有指征行宫腔镜下子宫纵隔切除术,术后2次妊娠均为自然受孕,也提示宫腔镜下子宫纵隔切除术可能改善了本例患者的妊娠率。
2.2.2 SU患者的孕产期管理
2019年加拿大妇产科学会将宫颈功能不全定义为:妊娠中期宫颈在无宫缩或无分娩发动,又或上述两者皆存在的情况下,宫颈的形态及功能无法维持妊娠顺利进行,是复发性妊娠中晚期流产及早产的重要原因[13]。作为临床诊断性疾病,宫颈功能不全缺乏客观的诊断标准,主要依据病史、体格检查及超声进行诊断。而宫颈环扎术是目前治疗宫颈功能不全的唯一术式和有效方法。
CUA患者作为妊娠期发生宫颈功能不全的高危人群,文献报道CUA合并宫颈功能不全的发病率可达30%以上[14]。有学者认为,CUA患者宫颈肌肉成分增加,结缔组织减少,妊娠期宫颈不足以对抗不断增加的不对称的宫腔压力,从而导致流产、早产[15]。2018年Mastrolia等[16]的队列研究结果显示,CUA与宫颈功能不全的发生呈独立相关。妊娠前宫颈功能评估结果(扩宫条通过7号无阻力)对CUA患者诊断宫颈功能不全有较高的参考意义。妊娠期应定期经阴道超声测量宫颈长度,宫颈长度<25 mm的患者应考虑选择宫颈环扎术[13]。Seidman等[17]的研究显示,对CUA并宫颈功能不全的患者孕期行宫颈环扎术可显著改善新生儿结局。2012年Chifan等[18]用超声监测316例CUA患者的宫颈长度,49例发生宫颈功能不全,其中SU 30例,双角子宫11例,单角子宫8例;对漏斗型宫颈及宫口开大<4 cm的患者行宫颈环扎术,术后继续定期监测超声,研究中的所有宫颈环扎术患者均发生早产(孕28~35周),其中SU平均分娩孕周约为32周。Golan等[14]对98例妊娠前诊断为CUA的患者行宫颈环扎术,术后产科结局明显改善,宫颈环扎术组足月分娩率从26%增加到63%。早产和延迟流产率从74%下降到37%,即使没有确诊宫颈功能不全的CUA患者宫颈环扎术后足月分娩率也从64%增加到96%,提前终止妊娠率从35.6%下降到4%。同样,国内文献报道也显示出宫颈环扎术对改善CUA患者妊娠结局有积极意义[19-20]。
行宫颈环扎术的患者定期门诊随访及增加产检频率尤为重要。定期超声监测宫颈长度变化,观察环扎线是否异位、宫颈是否撕裂或坏死等,建议每2周进行1次宫颈变化情况的评估,正常宫颈长度变化<0.5 mm/周,而宫颈功能不全患者宫颈长度变化约0.5~8.0 mm/周[21],必要时可根据宫颈变化情况调整超声评估时间,如宫颈进行性扩张(伴或不伴羊膜囊突出)应及时入院留观。同时,环扎缝线作为阴道异物,在提供机械屏障的同时也易导致宫颈黏液栓丢失。应定期行阴道分泌物培养及感染指标的监测,及时抗感染治疗[局部用药和(或)静脉用药]有利于避免生殖道上行感染导致的流产、早产甚至胎死宫内的风险。另外,宫颈功能不全患者活动量减少,定期评估血栓风险及时预防性抗凝治疗也是有必要的。
需特别注意的是,CUA合并宫颈功能不全者如有临产征象需密切观察,适时拆线,对产程中转剖宫产的评估、产道裂伤和产后出血的预防等均需有经验的医师参与,也主张适当放宽剖宫产指征。2019年的一项回顾性队列研究显示,SU患者妊娠前行宫腔镜下子宫纵隔切除术组与非CUA孕妇相比,表现出更高的剖宫产率(56.1% vs. 27.7%,P=0.000 2)及臀位发生率(19.5% vs. 6.8%,P=0.007)[22]。
阴道纵隔最常见于有SU的妇女,大多无症状,通常在常规检查或分娩过程中偶然发现。阴道纵隔并不是阴道分娩禁忌,因为SU妇女在分娩过程中纵隔可自行分开或经其中一侧阴道娩出,如产程中因阴道纵隔导致产程延长或停滞,也可根据情况行纵隔切开助产,或根据病情可适当放宽剖宫产指征,但分娩后应注意胎盘胎膜是否娩出完整,是否存在胎盘植入等并发症,尤其对于妊娠前行子宫纵隔切除术的患者。
2.3 本例的诊治体会
本例患者宫颈功能不全的高危因素包括:完全性SU,有宫腔操作史,中孕(24周)流产1次,妊娠前宫颈9号扩宫棒通过无阻力,临床可诊断宫颈功能不全,孕14周行预防性宫颈环扎术,发现左侧宫颈发育较右侧好,双侧宫颈功能不全,予MB66环扎线于左侧宫颈行双层环扎,右侧宫颈单层环扎。术后密切随访并积极抗早产治疗,于孕30+1周出现规律宫缩,早产难以避免,及时拆线,拆线后11 h早产顺产,胎儿由左侧宫颈及同侧阴道娩出,无胎盘植入、产道裂伤和产后出血等不良并发症发生,并抱活婴回家,提示宫颈环扎术确实起到延长孕周达6周的作用(第1次孕24周流产),可改善妊娠结局,而术后规范性的管理对延长孕周的作用也是值得肯定的。另外,妊娠期观察到右侧宫颈发育更好,羊膜囊突出更明显,而分娩时胎儿却从左侧宫颈娩出,可能为正式临产后,右侧子宫肌力更强,缩复作用使胎儿从弱肌力的左侧宫颈娩出。
综上所述,对不孕和妊娠中期流产的妇女,需特别注意子宫畸形的排查和宫颈功能不全的诊断,纳入高危妊娠进行围生期管理:完全性SU患者妊娠前行宫腔镜下子宫纵隔切除术可能改善妊娠成功率,诊断宫颈功能不全者,主张妊娠期行预防性宫颈环扎术并加强随访,对感染、早产、栓塞等并发症早期诊断并及时调整综合治疗方案,围分娩期及时拆除环扎线,密切母胎监护,适当放宽剖宫产指征并预防产后出血,母婴可获得良好预后。
参考文献
Overdiagnosis, overdetection, and overdefinition of the septate uterus: reexamination of the ASRM and ESHRE-ESGE criteria is urgently needed
[J].DOI:S0015-0282(19)30483-2 PMID:31371057 [本文引用: 1]
The presentation and management of complex female genital malformations
[J].DOI:10.1093/humupd/dmv048 URL [本文引用: 1]
Septate uterus according to ESHRE/ESGE, ASRM and CUME definitions: association with infertility and miscarriage, cost and warnings for women and healthcare systems
[J].
DOI:10.1002/uog.20291
PMID:30977223
[本文引用: 1]

To estimate the differences in frequency of diagnosis of septate uterus using three different definitions and determine whether these differences are significant in clinical practice, and to examine the association between diagnosis of septate uterus, using each of the three definitions, and infertility and/or previous miscarriage as well as the cost of allocation to surgery.This was a secondary analysis of data from a prospective study of 261 consecutive women of reproductive age attending a private clinic focused on the diagnosis and treatment of congenital uterine malformations. Reanalysis of the datasets was performed according to three different means of defining septate uterus: following the recommendations of the American Society for Reproductive Medicine (ASRM), a 2016 update of those of the American Fertility Society from 1988 (ASRM-2016: internal fundal indentation depth ≥ 1.5 cm, angle of internal indentation < 90° and external indentation depth < 1 cm); following the recommendations of the European Society of Human Reproduction and Embryology/European Society for Gynaecological Endoscopy (ESHRE/ESGE), published in 2013 and reaffirmed in 2016 (ESHRE/ESGE-2016: internal fundal/uterine indentation depth > 50% of uterine-wall thickness and external indentation depth < 50% of uterine-wall thickness, with uterine-wall thickness measured above interostial/intercornual line); and using a definition published last year which was based on the decision made most often by a group of experts (Congenital Uterine Malformation by Experts; CUME) (CUME-2018: internal fundal indentation depth ≥ 1 cm and external fundal indentation depth < 1 cm). We compared the rate of diagnosis of septate uterus using each of these three definitions and, for each, we estimated the association between the diagnosis and infertility and/or previous miscarriage, and anticipated the costs associated with their implementation using a guesstimation method.Although 32.6% (85/261) of the subjects met the criteria for one of the three definitions of septate uterus, only 2.7% (7/261) of them were defined as having septate uterus according to all three definitions. We diagnosed significantly more cases of septate uterus using ESHRE/ESGE-2016 than using ASRM-2016 (31% vs 5%, relative risk (RR) = 6.7, P < 0.0001) or CUME-2018 (31% vs 12%, RR = 2.6, P < 0.0001) criteria. We also observed frequent cases that could not be classified definitively by ASRM-2016 (gray zone: neither normal/arcuate nor septate; 6.5%). There were no significant differences (P > 0.05) in the prevalence of septate uterus in women with vs those without infertility according to ASRM-2016 (5% vs 4%), ESHRE/ESGE-2016 (35% vs 28%) or CUME-2018 (11% vs 12%). Septate uterus was diagnosed significantly more frequently in women with vs those without previous miscarriage according to ASRM-2016 (11% vs 3%; P = 0.04) and CUME-2018 (22 vs 10%; P = 0.04), but not according to ESHRE/ESGE-2016 (42% vs 28%; P = 0.8) criteria. Our calculations showed that global costs to the healthcare system would be highly dependent on the criteria used in the clinical setting to define septate uterus, with the costs associated with the ESHRE/ESGE-2016 definition potentially being an extra US$ 100-200 billion over 5 years in comparison to ASRM-2016 and CUME-2018 definitions.The prevalence of septate uterus according to ESHRE/ESGE-2016, ASRM-2016 and CUME-2018 definitions differs considerably. An important limitation of the ASRM classification, which needs to be addressed, is the high proportion of unclassifiable cases originally named, by us, the 'gray zone'. The high rate of overdiagnosis of septate uterus according to ESHRE/ESGE-2016 may lead to unnecessary surgery and therefore unnecessary risk in these women and may impose a considerable financial burden on healthcare systems. Efforts to define clinically meaningful and universally applicable criteria for the diagnosis of septate uterus should be encouraged. Copyright © 2019 ISUOG. Published by John Wiley & Sons Ltd.Copyright © 2019 ISUOG. Published by John Wiley & Sons Ltd.
Müllerian Duct Anomalies: Role in Fertility and Pregnancy
[J].DOI:10.1148/rg.2021210022 URL [本文引用: 1]
Reproductive outcomes in women with congenital uterine anomalies: a systematic review
[J].
DOI:10.1002/uog.10056
PMID:21830244
[本文引用: 1]

Congenital uterine anomalies are common but their effect on reproductive outcome is unclear. We conducted a systematic review to evaluate the association between different types of congenital uterine anomaly and various reproductive outcomes.Searches were performed using MEDLINE, EMBASE, the Cochrane Library and Web of Science. The Newcastle-Ottawa Quality Assessment Scale was used for quality assessment. Uterine defects were grouped into arcuate uteri, canalization defects (septate and subseptate uteri) and unification defects (unicornuate, bicornuate and didelphys uteri). Pooled risk ratios (RR) with 95% confidence intervals (CI) were computed using random effects models.We identified nine studies comprising 3805 women. Meta-analysis showed that arcuate uteri were associated with increased rates of second-trimester miscarriage (RR, 2.39; 95% CI, 1.33-4.27, P = 0.003) and fetal malpresentation at delivery (RR, 2.53; 95% CI, 1.54-4.18; P < 0.001). Canalization defects were associated with reduced clinical pregnancy rates (RR, 0.86; 95% CI, 0.77-0.96; P = 0.009) and increased rates of first-trimester miscarriage (RR, 2.89; 95% CI; 2.02-4.14; P < 0.001), preterm birth (RR, 2.14; 95% CI, 1.48-3.11; P < 0.001) and fetal malpresentation (RR, 6.24; 95% CI, 4.05-9.62; P < 0.001). Unification defects were associated with increased rates of preterm birth (RR, 2.97; 95% CI, 2.08-4.23; P < 0.001) and fetal malpresentation (RR, 3.87; 95% CI, 2.42-6.18; P < 0.001).Canalization defects reduce fertility and increase rates of miscarriage and preterm delivery. None of the unification defects reduces fertility but some are associated with miscarriage and preterm delivery. Arcuate uteri are specifically associated with second-trimester miscarriage. All uterine anomalies increase the chance of fetal malpresentation at delivery.Copyright © 2011 ISUOG. Published by John Wiley & Sons, Ltd.
Obstetric Complications in Women With Congenital Uterine Anomalies According to the 2013 European Society of Human Reproduction and Embryology and the European Society for Gynaecological Endoscopy Classification: A Systematic Review and Meta-analysis
[J].DOI:10.1097/AOG.0000000000004627 URL [本文引用: 1]
Reproductive, Obstetric and Neonatal Outcomes in Women with Congenital Uterine Anomalies: A Systematic Review and Meta-Analysis
[J].DOI:10.3390/jcm10214797 URL [本文引用: 1]
Type of congenital uterine anomaly and adverse pregnancy outcomes
[J].DOI:10.3109/14767058.2013.847082 URL [本文引用: 1]
Reproductive Implications and Management of Congenital Uterine Anomalies: Scientific Impact Paper No. 62 November 2019
[J].DOI:10.1111/1471-0528.15968 [本文引用: 1]
Management of congenital uterine abnormalities
[J].
DOI:10.1016/j.rbmo.2011.02.008
PMID:21652266
[本文引用: 1]

Congenital uterine abnormalities are a heterogeneous group of uterine configurations that may adversely affect reproductive potential. Although subtle variations can occur, the more common abnormalities fall into two broad categories of unilateral development or failure of midline fusion. These abnormalities have been well described for over a century although the mechanisms of their unfavourable impact on fertility and clinical management have not been systematically studied until recently. The quality of the literature on this topic has traditionally fallen below the level on which solid evidence-based decisions can be made. Nonetheless, considerable progress has been made in recent times. The understanding of the aetiology of these abnormalities and how they impact reproduction has matured and evolved and this evolution and the growing body of recent studies better define clinical scenarios in which intervention will clearly and positively impact outcome. This article will review four common congenital abnormalities, their impact on reproduction, options for management and the role of assisted reproduction treatment in maximizing reproductive potential. Recommendations are made with consideration of the quality of the literature in an outcome-driven environment.Copyright © 2011 Reproductive Healthcare Ltd. Published by Elsevier Ltd. All rights reserved.
Septum resection for women of reproductive age with a septate uterus
[J].DOI:10.1002/14651858.CD008576.pub4 [本文引用: 1]
Clinical implications of congenital uterine anomalies: a meta-analysis of comparative studies
[J].DOI:10.1016/j.rbmo.2014.09.006 URL [本文引用: 1]
No. 373-Cervical Insufficiency and Cervical Cerclage
[J].DOI:10.1016/j.jogc.2018.08.009 URL [本文引用: 2]
Cervical cerclage--its role in the pregnant anomalous uterus
[J].Twenty-nine cases of cervical incompetence were found among 98 women diagnosed as having a congenital uterine anomaly on hysterosalpingography, a high incidence of 30%. The highest incidence was found in the bicornuate uterus group--38%. The incidence of premature delivery and late abortion was higher in this group than in the rest of the patients with uterine anomalies (55% and 68%, vs. 45% and 32%). An obvious improvement in obstetrical performance was noted after cerclage. In the cervical incompetence group, term deliveries increased from 26% to 63%. Premature deliveries and late abortions dropped from 74% to 37%. Even in the patients with anomalous uterus without proven diagnosis of cervical incompetence, term deliveries increased from 64% to 96%, and pregnancies terminating prematurely dropped from 35.6% to 4%, following cerclage. No doubt exists as to the need for cerclage in cases of cervical incompetence. We also believe it should be performed prophylactically in cases of bicornuate uterus. The concept of routine prophylactic cerclage in all cases of uterine anomalies should be considered.
Congenital uterine malformations as indication for cervical suture (cerclage) in habitual abortion and premature delivery
[J].
DOI:10.1016/0090-8258(83)90067-7
PMID:6140235
[本文引用: 1]

Fifteen women with diminished fertility as a result of congenital uterine anomalies were treated by cervical suture (cerclage) in the 11th-12th week of pregnancy without surgical correction of the uterine anomaly. None of these women had either clinical or radiological evidence of cervical incompetence. As a result of the treatment, 13 of the women delivered live full-term mature infants. None of the women aborted, only two women delivered prematurely, and both infants were alive and well. Comparison of these good results to the very poor outcome of previous pregnancies in these women points to a distinct advantage to be gained by cervical suture. As a result of this experience, we recommend cervical suture in cases of diminished fertility as a result of congenital uterine anomaly. We recommend that the suture be performed before considering surgical repair of the anomaly and irrespective of lack of evidence of cervical incompetence. Only in cases where cervical suture is unsuccessful, would we recommend surgical correction according to the accepted techniques.
Independent association between uterine malformations and cervical insufficiency: a retrospective population-based cohort study
[J].DOI:10.1007/s00404-018-4663-2 URL [本文引用: 1]
The role of cervical cerclage in the management of uterine anomalies
[J].
Cervical incompetence associated with congenital uterine malformations
[J].Cervical incompetence is basically a cervix that is too weak to stay closed during a pregnancy. It is generally categorized as premature opening of the cervix without labor or contractions.To estimate the incidence of incompetence of the uterine cervix at patients with congenital uterine malformations.Our study was a retrospective and prospective one between 2002 and 2009. We evaluate the length of the cervix by transvaginal ultrasonography during the second trimester of pregnancy.We had 316 cases with congenital uterine malformations. From these we found 49 (15.3%) women with incompetence of the cervix: 8 (2.5%) with unicornuate uterus, 11 (3.4%) with bicornuate uterus and 30 (9.5%) cases uterus with septum. For all these wad made cerclage when we found funneling of the cervix or the cervix was open less than 4 cm. The use of ultrasonography has been very helpful with the diagnosis, and is made when the cervical os (opening) is greater than 2.5 cm, or the length has shortened to less than 20 mm. All patients had preterm delivery.When we have cases with congenital uterine malformations we must think that incompetence of the cervix could be associated, so we must assess the status of the cervix for these patients by serial ultrasound examinations starting between 16 and 20 weeks of gestation. Our patients had preterm delivery caused not only the incompetent cervix, but the malformation of the uterus is implicated also.
宫腹腔镜完全双角子宫成形术后宫颈环扎成功分娩一例
[J].DOI:10.3969/j.issn.1674-1870.2016.06.013 [本文引用: 1]
单角子宫妊娠合并宫颈机能不全一例并文献复习
[J].DOI:10.3969/j.issn.1674-1870.2020.05.026 [本文引用: 1]
No. 257-Ultrasonographic Cervical Length Assessment in Predicting Preterm Birth in Singleton Pregnancies
[J].DOI:10.1016/j.jogc.2017.11.016 URL [本文引用: 1]
Is hysteroscopic metroplasty using the incision method for septate uterus a risk factor for adverse obstetric outcomes?
[J].DOI:10.1111/jog.13884 URL [本文引用: 1]