间皮囊肿是良性囊性间皮瘤的一种组织类型,其组织来源于覆盖浆膜腔表面的间皮细胞,囊壁很薄,无明显间皮组织增生,囊内衬覆分化良好的扁平间皮。间皮囊肿可发生于任何间皮覆盖区域,如肠系膜、大网膜、胸腔纵隔、子宫圆韧带及附件等,主要累及盆腹腔腹膜,较少发生于子宫[1]。2010年6月—2021年3月南京医科大学第一附属医院(我院)收治了良性间皮囊肿患者30例,发生于子宫者仅4例,除本文报告病例外,其余3例均为剖宫产术中意外发现。子宫间皮囊肿缺乏典型的临床表现,多以腹部包块就诊,或在其他腹腔手术时意外发现,术前诊断困难,极易误诊为子宫肌瘤囊性变或附件囊肿。现报告我院妇科收治的1例子宫间皮囊肿术前误诊为子宫肌瘤囊性变的病例,并复习国内外文献,就该病的发病机制、诊断与鉴别诊断及治疗进行总结探讨,以期为子宫间皮囊肿的临床诊疗提供依据。
1 病例报告
1.1 我院收治间皮囊肿患者的发病部位
2010年6月—2021年3月我院共收治30例良性间皮囊肿患者,平均年龄(47±16)岁,女性25例(83.3%),发病部位分别为附件40%(12/30)、盆腹腔来源不明确23.3%(7/30)、胸腔纵隔16.7%(5/30)、子宫13.3%(4/30)、大网膜3.3%(1/30)及膀胱3.3%(1/30)。见表1。
表1 2010年6月—2021年3月我院收治的间皮囊肿患者发病部位
| 发病部位 | 例数(例) | 占比(%) | 男(例) | 女(例) | 年龄(岁) |
|---|---|---|---|---|---|
| 附件 | 12 | 40.0 | 0 | 12 | 48±20 |
| 胸腔纵隔 | 5 | 16.7 | 2 | 3 | 55±18 |
| 子宫 | 4 | 13.3 | 0 | 4 | 44±8 |
| 腹腔-来源不明确 | 4 | 13.3 | 2 | 2 | 45±2 |
| 盆腔-来源不明确 | 3 | 10.0 | 1 | 2 | 42±17 |
| 大网膜 | 1 | 3.3 | 0 | 1 | 47 |
| 膀胱 | 1 | 3.3 | 0 | 1 | 34 |
| 合计 | 30 | 100.0 | 5 | 25 | 47±16 |
1.2 本病例情况
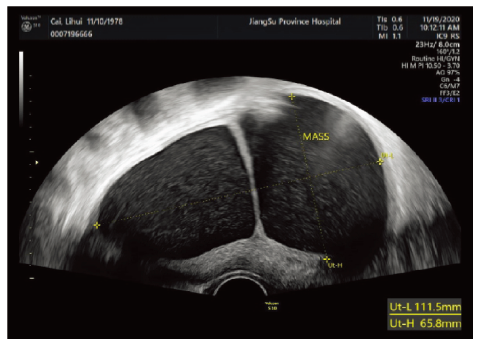
患者 女,42岁,因发现盆腔囊肿1年半,于2020年11月18日收治我院妇科。患者平素月经规律,无痛经。孕4产1,2002年足月剖宫产娩一健康男婴,3次流产均为社会因素在妊娠40 d左右药物流产或人工流产,具体年份不详。2019年5月在外院体检发现盆腔囊肿,大小不详。2019年9月15日就诊于我院妇科门诊,盆腔B超示:子宫右前壁见9.2 cm×6 cm×7 cm囊性包块,凸向浆膜下。建议手术治疗,患者拒绝。2020年9月20日患者于我院妇科门诊复诊,B超示(见图1):子宫右前壁见11.2 cm×6.6 cm×7.1 mm囊性暗区,向外突出,内见分隔及细密点絮状回声,分隔上探及少许血流信号。再次建议患者手术治疗,因工作原因,患者推迟至2020年11月18日入院治疗。
图1
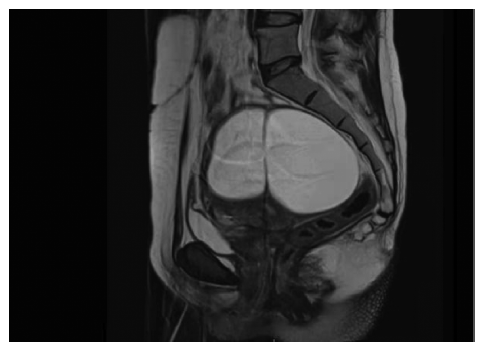
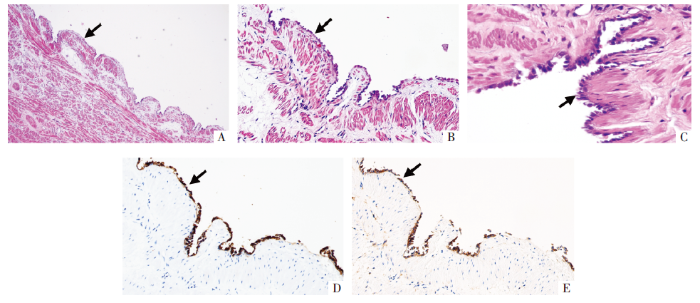
入院查体:盆腔内触及直径约11 cm囊性包块,张力大,活动好,无压痛,与子宫及双侧附件分界不清。2020年11月19日查肿瘤标志物示:糖类抗原72-4(carbohydrate antigen 72-4,CA72-4)为46.52 U/mL,CA125、CA19-9、甲胎蛋白(alpha fetoprotein,AFP)、癌胚抗原(carcinoembryonic antigen,CEA)及人附睾蛋白4(human epididymis protein 4,HE4)均未见异常。2020年11月21日盆腔磁共振成像(magnetic resonance imaging,MRI)示(见图2):子宫右前壁膨隆,见囊状异常信号肿块影,大小约11.1 cm×6.3 cm×6.1 cm,考虑子宫肌瘤囊性变。初步诊断:盆腔肿物(子宫肌瘤囊性变?)。2020年11月24日行剖腹探查术,术中见:子宫不规则增大如妊娠3个月,前壁及宫底均呈囊性凸起,囊壁薄,双附件未见异常。按照患者及其家属术前意愿行全子宫+双侧输卵管切除术。术毕剖视子宫见子宫前壁及宫底2个囊腔,囊液清亮淡黄色,囊壁光滑,囊腔周围子宫肌层组织少(见图3和图4)。术后病理示:(子宫)符合间皮囊肿,2个囊腔大小分别为3.5 cm×3 cm×2 cm和4 cm×3 cm×2.5 cm。免疫组织化学染色提示(子宫)囊壁被覆上皮:GATA3阴性,配对盒基因8(pair box-8,Pax-8)阳性,肾母细胞瘤基因1(Wilm′s tumour gene-1,WT-1)阳性,间皮细胞阳性,D2-40阳性,CD31阴性,天冬氨酸肽酶A(Napsin A)阴性,结合苏木精-伊红(Hematoxylin-Eosin,HE)染色切片(见图5),本病例诊断为子宫间皮囊肿。患者术后恢复好,随访至2021年11月无异常。
图2
图3
图4
图5
图5
HE及免疫组织化学染色图片
注:A HE×40,B HE×200,C HE×400,箭头所示为囊壁内覆衬单层立方形间皮细胞。D 囊壁被覆上皮间皮细胞呈阳性(SP法×200),E 囊壁被覆上皮D2-40呈阳性(SP法×200),箭头所示为囊壁被覆上皮免疫标志处。
2 讨论
2.1 间皮囊肿的定义
间皮囊肿与多囊性间皮瘤被认为是良性囊性间皮瘤的两种不同类型,因两者在组织病理学上有诸多相似之处,很多报道中将两者混为一谈,但事实上两者在大体外观及生物学行为上有很多不同之处。间皮囊肿被认为是真正的包涵性囊肿,而不是恶性肿瘤,囊肿较小,通常<5 cm,单发,又被称为孤立性间皮囊肿,常为单房,可为2~3个囊腔,囊壁很薄,囊内衬覆分化较好的扁平间皮细胞,无明显间皮增生[6]。而世界卫生组织软组织肿瘤分类将多囊性间皮瘤列入良性及低度恶性间皮瘤[7]。目前对于这类肿瘤的认识较为混乱,有观点认为是包涵性或反应性增生,有部分学者认为是良性肿瘤,亦有部分学者认为其是可侵及肝、脾及胰的低度恶性肿瘤,因此这类肿瘤名称混杂——囊性间皮瘤、腹膜炎性囊肿、多囊性腹膜间皮瘤、手术后腹膜囊肿及多囊性腹膜包涵囊肿等[6⇓-8]。结合本例患者术前影像、大体标本及术后病理,符合子宫孤立性多房间皮囊肿。
2.2 子宫间皮囊肿的发病机制
2.3 子宫间皮囊肿的诊断与鉴别诊断
子宫间皮囊肿的术前诊断较为困难,因患者常无特异性的临床表现,多数以盆腹腔包块首诊,仅少数患者有月经过多的临床表现,影像学及实验室检查亦缺乏特异性,术前易误诊为子宫肌瘤囊性变、卵巢囊肿、盆腹腔炎性包裹性积液和盆腔囊性淋巴瘤等。本例患者亦无典型临床表现,术前误诊为肌瘤囊性变,回顾性分析术前影像资料,B超示子宫右前壁囊性暗区,囊内见细密点絮状回声,内见分隔。MRI示肌壁间囊性包块内部信号均匀,T1加权成像(T1 weighted imaging,T1WI)呈低信号,T2加权成像(T2 weighted imaging,T2WI)呈高信号,弥散加权成像未受限,囊壁菲薄、增强扫描囊壁及分隔明显强化,强化程度与肌层相当。首先通过影像学明确囊肿位置位于子宫体而非卵巢,彩色多普勒超声未提示囊壁上丰富血流信号,MRI提示囊壁强化与肌层相当,则提示良性病变可能性较大。子宫肌瘤囊性变因变性部分为液体,超声图像上常表现大小不等的无回声区,或相互融合为较大的囊腔。而其在MRI中T1WI呈低信号,T2WI呈高信号,与子宫间皮囊肿难以鉴别,但子宫肌瘤囊性变通常囊壁较厚[10-11],而子宫间皮囊肿囊壁菲薄。因妇科及影像学医师缺乏对子宫间皮囊肿的认识,本例患者术前误诊为子宫肌瘤囊性变。因此影像学和妇科医师应加强对该病的了解,对术前明确诊断具有重要意义。
目前确诊间皮囊肿的唯一方法是术后病理,镜下一般见被覆单层立方上皮,很少有复层,不增生,细胞核和细胞质比例适中,无核分裂,细胞极向正常,可通过免疫组织化学染色间皮标志Pax-8、WT-1、间皮细胞、D2-40和钙视网膜蛋白等阳性进行辅助鉴别。而子宫肌瘤囊性变囊壁内层无上皮覆盖,囊壁细胞符合梭形细胞病变,可通过免疫组织化学染色平滑肌标志平滑肌肌动蛋白、结蛋白和高分子量钙结合蛋白等阳性辅助鉴别。既往有学者报道将细针穿刺用于术前确诊间皮囊肿成功的案例,但因其取材的盲目性和局限性,结果往往为反应性间皮细胞,无特异性诊断价值。并且在性质不明的情况下进行穿刺,一旦盆腔囊肿为恶性,易造成肿瘤播散种植,严重影响预后[12-13]。
2.4 子宫间皮囊肿的治疗及预后
子宫间皮囊肿临床罕见,目前尚无明确的治疗指南。有学者认为因其良性病变的性质,在诊断明确的情况下可保守治疗,严密随访。但临床实践中,由于缺乏特异性的实验室及影像学检查手段,术前很难明确病变性质,因此,手术切除仍然是首选的治疗方式。由于间皮囊肿囊壁菲薄、多囊腔、边界不清,增加了囊肿完整剥除的手术难度,继而会增加术后复发的风险,因此对于年龄较大、无生育要求的患者,全子宫切除是较为彻底的手术方式。本例患者的术前诊断是子宫肌瘤囊性变,患者42岁,无生育要求,影像学检查提示子宫瘤变体积较大,和患者沟通后选取的手术方式是全子宫切除术。术中见子宫前壁及宫底两个较大囊腔,囊壁极薄,囊壁与正常子宫肌层分界不清,囊壁周围肌层组织少。如行囊壁剥除,将出现两个问题,一是囊壁难以和正常的肌层分离,二是子宫难以重塑成形或缝合后宫底肌层菲薄。该病例提示对于术前影像学检查诊断为子宫肌瘤囊性变的患者,还需要警惕子宫间皮囊肿的可能。尤其是年轻和需要保留子宫的间皮囊肿患者,术中存在囊壁剥离困难或子宫难以重塑成形的可能,术前应充分沟通,取得患者及家属的充分知晓和理解。
综上所述,子宫间皮囊肿发病率极低,妇科医师和影像学医师对其认识有限,易误诊为子宫肌瘤囊性变。子宫间皮囊肿和子宫肌瘤囊性变虽然都是良性病变,但手术处理方式不尽相同。囊性变的肌瘤由于有假包膜易行肌瘤剔除术,而子宫间皮囊肿与子宫肌层分界不清,剥离困难,增加了病灶残留和术后复发风险。因此,对于临床高度疑诊子宫间皮囊肿的患者,手术方式的选择应充分考虑患者年龄、生育需求、病灶残留和术后复发的风险,对于采取囊肿剥除术的患者,术后应严密随访。
参考文献
Benign Cystic Mesothelioma of Uterus: An Unusual Cause of Pelvic Pain
[J].DOI:10.1007/s13224-016-0917-8 URL [本文引用: 1]
Mesothelial cyst of uterine corpus misdiagnosed as leiomyoma
[J].DOI:10.1097/CM9.0000000000000291 [本文引用: 1]
子宫浆膜下间皮囊肿误诊附件包块的临床分析
[J].DOI:10.3870/j.issn.1672-0741.2004.05.041 [本文引用: 1]
WHO classification of tumours
WHO classification of tumours
Multicystic mesothelioma caused by endometriosis: 2 case reports and review of the literature
[J].
DOI:10.1097/PGP.0b013e3181f99def
PMID:21293283
[本文引用: 1]

Multicystic mesothelioma was described as a benign neoplasm in most reports. But, whether it is neoplastic or reactive is still controversial. Although multicystic mesothelioma is often accompanied by endometriosis, histologic findings of the lesion with endometriosis have not been well documented. In this report, 2 cases of multicystic mesothelioma with endometriosis were studied histologically. The first lesion consisted of multiple cysts having thin walls lined with single-layered cuboidal mesothelia, and in the cystic walls, small foci of endometriosis were found. The second lesion was next to the endometriotic cysts in the pelvic space. These histologic findings suggest that endometriosis greatly contributes to the origin of the lesions. In addition, from the review of the literature, cystic mesothelioma was divided into 2 categories, that is, neoplastic or non-neoplastic lesions. Differentiation of both disorders might be possible by the following: size of the lesion, macroscopic and microscopic solid proliferation, features of adenomatoid tumor, and common mesothelioma-like histology. In conclusion, multicystic mesothelioma accompanied by endometriosis is thought to be a secondary non-neoplastic lesion induced by adhesion or inflammation rather than a neoplasm.
磁共振DWI联合ADC对子宫肉瘤和变性子宫肌瘤的诊断价值
[J].DOI:10.3969/j.issn.1671-8348.2019.14.019 [本文引用: 1]
What MRI features suspect malignant pure mesenchymal uterine tumors rather than uterine leiomyoma with cystic degeneration?
[J].DOI:10.3802/jgo.2018.29.e26 URL [本文引用: 1]
Benign multicystic peritoneal mesothelioma: a case report
[J].DOI:10.1186/1752-1947-4-385 URL [本文引用: 1]
Cystic peritoneal mesothelioma: report of a case
[J].
DOI:10.1007/s00595-010-4301-5
PMID:21191708
[本文引用: 1]

Benign multicystic peritoneal mesothelioma (BMPM) is a rare disease with good short-term prognosis and rare malignant transformation. However, its biological significance remains unexplained. A neoplastic origin is considered by many authors to require a surgical excision, based on the high recurrence and progressive growth rate of the tumors. However, alternative or integrative treatment options have also been proposed. A 45-year-old woman presented to our unit with a history of occasional discomfort and pain in the left hip. On physical examination, we noticed a tough-elastic, fixed mass located in the iliac fossa. Computed tomography scan detected a mass with multiseptated cystic-like areas. Due to the similarity of these findings to a primitive sarcomatous tumor of the retroperitoneum, an arteriographic study was also performed. The patient underwent en bloc resection of the mass, including a segment of the sigmoid colon. The final pathologic diagnosis was cystic mesothelioma. Further studies are needed to better understand the etiology and pathogenesis of this rare disease, and to define a more tailored treatment plan.
Mesothelial cyst of the round ligament misdiagnosed as irreducible inguinal hernia
[J].DOI:10.1155/2013/408078 [本文引用: 1]
Mesothelial Cysts
[J].
DOI:10.1093/ajcp/aqaa189
PMID:33258870
[本文引用: 1]

Peritoneal mesothelial cysts have been reported under various terms, including benign cystic mesothelioma, usually in the form of case reports/series, whereas extraperitoneal cases are rarely reported. Our objective was to report the detailed characteristics of cystic lesions of the serosal cavities.We retrospectively examined the clinicopathologic findings of a series of mesothelial cystic lesions (n = 79).Most cases (n = 68, 86%) concerned the peritoneum, whereas 11 (14%) concerned the pericardium. No pleural cases were found. A total of 51 (64.5%) lesions were solitary, whereas 28 (35.5%) were multiple. Peritoneal lesions harbored a plump eosinophilic mesothelium and a loose connective stroma, whereas pericardial lesions showed a cuboidal/flattened mesothelium, collagenous stroma, intense inflammation, and other tissue types, like adipose and muscle tissue. Solitary peritoneal lesions are usually extrapelvic and found in older patients incidentally during other surgeries, whereas multiple lesions are found in younger patients and usually in the pelvis. The lesions show a benign clinical course with rare recurrences but no malignant transformation.Most mesothelial cysts are peritoneal and rarely pericardial. Peritoneal cysts differ from pericardial cysts. Peritoneal solitary lesions differ from multiple lesions, also suggesting their pathogenetic differences.© American Society for Clinical Pathology, 2020. All rights reserved. For permissions, please e-mail: journals.permissions@oup.com.